Sperm storage (sperm banking)
A patient may be referred for sperm storage if they are at risk of losing their fertility. This may be due to illness, surgery, treatments such as chemotherapy, radiotherapy or gender reassignment, or to preserve sperm obtained through surgical sperm retrieval.
The sperm storage process
The process of sperm storage starts with a consultation with a Fertility Scientist to discuss the sperm storage procedure and complete all necessary consent forms.
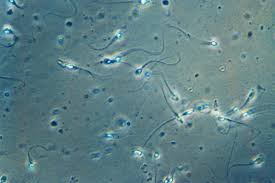
At this first appointment, the patient is asked to produce a semen sample. A Fertility Scientist will assess the quality of the sperm, and will freeze the sperm, which is then stored in liquid nitrogen at -196oC. The sperm is stored in 1ml ampoules, with an additional small ampoule stored for post thaw testing. The post thaw ampoule is thawed out in the weeks following the freeze and the sperm quality assessed to indicate how well the sperm survives the freeze/thaw process. The results of the post-thaw tests are sent to the referring doctor and the patient.
In order to maximise the number of ampoules of sperm in storage, the patient is asked to produce 2 further semen samples, each one after a period of 2-5 days abstinence.
Patients who have sperm frozen should be aware that:
- There is no guarantee of sperm quality if and when it is thawed.
- Illness at the time of freezing or prior to it could affect the number and quality of sperm.
- If the sperm are of poor quality, assisted conception procedures such as IVF or ICSI may be required to attempt to achieve a pregnancy in the future.
- Sperm is stored initially for a period of 10 years. Following this period, by completion of the necessary consent forms, storage may be extended in 10 year increments up to a maximum of 55 years.
- It will be necessary to screen any patient about to undergo sperm freezing for Hepatitis B, Hepatitis C and HIV. The semen will be held in quarantine until the results of the tests are available and will then be transferred into a suitable long term storage vessel.
Semen cross-contamination
Although screened semen will never knowingly be stored alongside infected semen, there is a slim chance that cross-contamination could occur while the semen is in the quarantine container. If a sample is stored for any amount of time alongside a sample known to be infected then the patient involved would be informed and would decide whether or not to use the sample.
It should be noted that the risk of cross-contamination is regarded as low. It should also be noted that the current system is not a full quarantine system but a screening system. A full quarantine system would involve a re-screen after 6 months before transfer from an individual quarantine flask. If you have any queries about this please contact a scientist at the Centre.
Change of patient details
Patients must ensure that they inform the unit of any change in their address or health status so that review of the storage may take place.